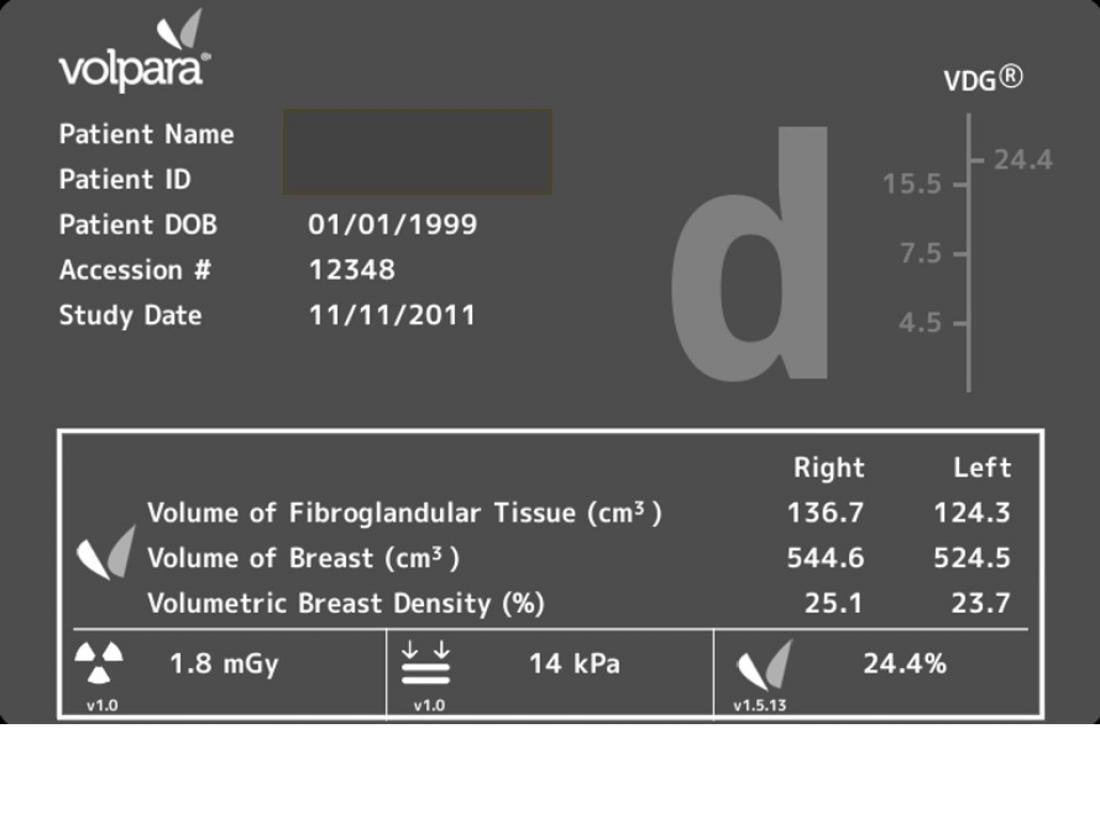
Volpara TM breast density assessment tool (screen capture showing the analysis from one patient)
“Breast density, assessed by mammography and expressed as a percentage of the mammogram occupied by radiologically dense fibroglandular tissue, is a strong predictor of the failure of mammographic screening to detect breast cancer lesions.” [Ng et al, Lancet Oncology, Vol. 13, April 2012]
There is a strong connection between breast cancer and the high rate of breast density. These are cases wherein the patient has previously undergone mammography screening and been cleared as ‘normal’. A subsequent diagnosis of cancer indicates the failure of mammography to detect the breast cancer.
The risk of breast cancer from high breast density is twice higher than other factors (except when a family history of the disease is present in women aged 40-49 years). Whether breast density is an independent risk factor or a stimulant to other cancer risk factors is still being debated.
University of Malaya researchers, Prof. Kwan Hoong NG and his team published two papers on this subject - “Standardisation of clinical breast-density measurement”, which highlights the need for standardised protocol in breast density measurement [Ng et al, Lancet Oncology, Vol. 13, April 2012], and “Vision 20/20: Mammographic Breast Density and its Clinical Applications”, a comprehensive review of breast density measurement over the past 40 years, as well as its current and future applications in breast cancer [Ng et al, Medical Physics 42:7059, 2015].
What is Breast Density?
During a mammogram, one breast is placed on a firm flat panel at a time. Another panel then applies pressure on the breast, resulting in compression of the breast between the two panels. Compression spreads out the breast tissue and eliminates motion, thus reducing chances of blurred images.
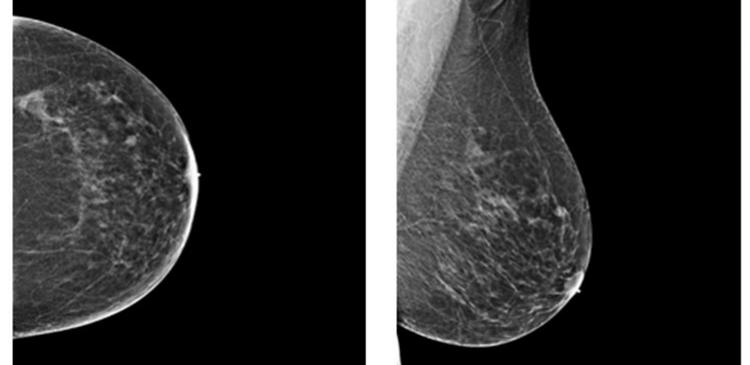
A radiologist will then determine the density of a woman’s breasts using the mammogram images. Dense tissue appears white on a mammogram and is composed of less fat but more fibroglandular tissue (connective tissue and epithelium). Since both dense and cancer tissues appear white on the mammography, it is possible that cancer lesions can be “masked” or hidden by dense tissue. The darker areas of a mammogram correspond to the less attenuating adipose (fatty) tissue. High breast density means a greater amount of breast and connective tissue as compared to fat.
The Connection to Breast Cancer and Risk Factors
Research has shown that women with dense breasts have a 4 to 6-fold increased risk of developing breast cancer. Age and the BRCA gene mutation carrier status further increase the relative risks involved. Even in comparison with the relative risks associated with a direct family history of the disease or any menstrual or reproductive risk factors, the relative risk of breast cancer associated with high breast density is substantially greater than such factors. 1-6
The Breast Cancer Facts & Figures 2011-2012 by American Cancer Society revealed that dense breasts are four times more likely to develop cancer than those of average density, and fatty breasts are around half as likely to develop cancer as compared to average density breasts.
Additionally, the National Cancer Institute (NCI) provides a list of current breast cancer risk prediction models, i.e. absolute risk prediction models, gene carrier status risk prediction models, and risk prediction models of women at high risk. These models help identify high-risk individuals of breast cancers, allowing for earlier or more frequent screening and counselling.
Absolute cancer risk is the probability that an individual with given risk factors and a given age will develop cancer over a defined period of time e.g. race, age, sex, genetics, body mass index, family history of cancer, history of tobacco use, use of aspirin and nonsteroidal anti-inflammatory drugs (NSAIDS), physical activity, use of hormone replacement therapy (HRT), reproductive factors, history of cancer screening, and dietary factors.
Gene carrier status risk prediction models estimate the likelihood of detecting a mutation in a cancer susceptibility gene (e.g., BRCA1 and BRCA2) in a given family or individual.
But in the breast density context, there is good news in sight. Breast density is a modifiable risk factor that can be addressed e.g. by following lifestyle parameters, food consumption (e.g. vegetables, vitamin D, calcium) and by the use of Tamoxifen.7
Measuring Breast Density: Radiologist Assessment, 2D Surface-Area Based & 3D Volumetric Breast Density
The challenge in assessing breast density, however, lies in the fact that there is no standard common understanding of breast density and there are currently many different ways of measuring it. [Ng et al, Lancet Oncology, Vol. 13, April 2012]
The Vision 20/20 article traced the development of breast density estimation from pattern analysis to area-based analysis and the current automated volumetric breast density (VBD) analysis. The initial link between breast density and cancer was reported by Professor John Wolfe and others on in the 1970s. Their work using breast tissue stratifications led them to suggest that certain density patterns were markedly more likely to develop breast cancer.
(a) Radiologist Assessment based on Classification Schemes
Usually, mammographic breast density is visually assessed by radiologists on the basis of several classification schemes; the most widely used being the Breast Imaging Reporting and Data System (BI-RADS), Boyd’s six category classification, and Tabar. The term ‘visually assessed’ indicates the inherent cause for concern. Such assessments are subjective and would depend upon the skill and experience of the reporting radiologist.
Mammograms have different appearances depending on how they are acquired. An experienced radiologist would be aware of circumstantial factors that affect any readings, such as the x-ray exposure used, adequacy of compression, and the exact positioning of the breast. In the hands of a less skilled radiologist, the results could vary greatly.
In 1993, the American College of Radiology (ACR) began a process to standardise breast density reporting in the 3rd edition of the BI-RADS dictionary. In 2013, given the increased attention on breast density reporting, the ACR decided to focus BI-RADS density on the risk of cancer being missed. In the 5th edition, the ACR reiterated that breast density is an assessment of the volume of dense tissue in the breast.
Classification of breast composition according to BI-RADS 5th edition:
a The breasts are almost entirely fatty.
b There are scattered areas of fibroglandular density.
c The breasts are heterogeneously dense, which may obscure small masses.
d The breasts are extremely dense, which lowers the sensitivity of mammography.
Indeed, the ACR explicitly notes in the 5th edition that subjective estimates from a 2D mammogram are imprecise indicators of volume.
The sensitivity of mammography has been shown to be as low as 48% in dense breasts (as compared to 98% in fatty breasts). Therefore, every second or third cancer may be missed in women with dense breasts8. Furthermore, an experiment involving the same woman imaged over 8 years on different x-ray systems revealed varying results of breast density.
(b) 2D Surface-Area Based
In the 1980s, intrigued by the work of Professor Wolfe, Professor Norman Boyd teamed up with Professor Martin Yaffe to develop Cumulus, a semi-automated density software based on visual area based density assessment.
This method of assessment utilizes planimetry, iterative thresholding and segmentation analysis. But with the development of semi-automated computerized methods, several notable radiologists have expressed concern that while radiologists can guess-estimate the percentage of dense breast tissue, they are using 2D (surface-area-based) information to assess 3D tissue. Therefore, they cannot be accurate in any absolute sense.
So what we have is the problem of looking at an x-ray or mammography (2D) and trying (via certain methods and analysis) to ascertain the volumetric ratio of dense fibroglandular tissue to the whole breast. The results are quantitative, semi-automated but still subjective (to some extent).
The semi-automated density software Cumulus is a promising research tool but limited in its clinical utility because of the time it takes. Subsequent attempts to reliably automate the density assessment have failed due to the variability in mammography systems, breast composition and image processing algorithms.
(c) 3D Volumetric Breast Density
In the Vision 20/20 article, the work quoted by Ralph Highnam, Ph.D., and Sir Professor Mike Brady on Volumetric Breast Density (VBD) has given much cause for hope. Volumetric Breast Density utilizes an objective approach based on the physics of the x-ray imaging process.
The results are quantitative, automated, objective and reproducible. To obtain a real, true physical measurement, objective measurements of breast density are used. It is independent of equipment (i.e. irrespective of different x-ray systems), exposure factors and radiographic technique. VBD provides absolute volumes (and areas) of the whole breast, dense tissue and adipose tissue. Further, it compares well to MRI and CT and correlates with visual BI-RADS.
Commercial software that measures volume density and can be used in addition to routine mammography is becoming available e.g. R2 QuantraTM (Hologic), VolparaTM (Matakina), Spectral (Philips) and M-Vu (VuComp) programs. Their robustness and acceptance by the international community have not been established, but merit investigation.
Volpara generates mathematical, computer-driven breast density measures based on the true 3D properties of a woman’s breasts using the calculation of the volume of fibroglandular tissue divided by the total volume of tissue within the breast. In addition to dozens of publications from leading research sites around the globe using VolparaDensity, the software has been validated against a subset of the 2006 DMIST study and in multiple independent studies against breast MRI measurements of fibroglandular volume.
Volumetric breast density is reproducible and easy to automate. Great improvement in VBD measurements is expected that will satisfy the needs of radiologists, epidemiologists, surgeons, and physicists.
Towards an International Standard Protocol for Assessing Breast Density
Breast density information is relevant in clinical decision-making for screening, diagnosis, intervention and the management of breast cancer. We need to have breast-density measurements that are standardized, reliable and reproducible. This will facilitate comparative analysis, more accurate risk prediction, and provide more tailored, strategic, cost-effective screening for breast cancer than is currently available.
Currently, breast density measurements have been used to track changes in density patterns which occur over time or with medical treatment, such as with Hormone Replacement Therapy (HRT). It’s also useful to assess the effectiveness of Tamoxifen on an individual.
In the long-term, with a standardized protocol in place, the monitoring of global and regional breast density changes over time can be tracked. This enables a better chance of detecting early signs of breast cancer. Additionally, health policy makers will be able to determine the screening age of individuals and save on treatment costs.
US Legislation and the ‘Are you Dense?’ Advocacy Movement
The importance of breast density and its link to cancer has caught the attention of US policymakers. The US Congress introduced the Mammography Quality Standards Act (MQSA) in 1992, and the Mammography Reporting Act of 2011. Modelled on the Breast Density Inform laws (Connecticut 2009, and Texas 2012), it requires physicians to provide information about a patient’s breast density in every mammography summary. Additionally, they are required to provide advice about the heightened risk faced by people with dense breasts and controversially - the supplemental screening procedures that could be of benefit. In 2012, the Breast Density and Mammography Reporting Act was enacted. As at August 2016, 28 states in America have adopted this legislation.
Working concurrently to raise awareness on the link between breast density and breast cancer, the Are You Dense? movement by Nancy M Cappello, Ph.D., seeks to ensure that women be informed of their breast density so that they understand the limitations of mammography screening and thereby decide to be imaged using another complementary modality.
Dr. Cappello’s passion as an advocate is the result of her own traumatic experience. In early 2004, she was diagnosed with advanced stage breast cancer. The diagnosis came after her 11th mammogram was reported as ‘normal’. Up until 2004, Dr. Cappello had diligently undergone annual mammograms. It was the first time she’d heard about breast density and realized that the mammography report details are not typically shared with patients. Dr. Cappello endured an aggressive treatment consisting of chemotherapy, radiation, numerous surgeries and hormone therapy.
Conclusion
Increased breast density is associated with a higher risk of breast cancer. Breast density is just one variable in the risk model (but a strong indicator). Whether reducing breast density also reduces cancer risk is a subject of debate. Most of the studies on breast density are based on a 2D mammogram. As such, we need to be cautious in using it as a predictor of breast cancer. We need to study volumetric information due to the 3D structure of the breast.
Mammography screening has been shown to have reduced sensitivity for the dense breast. This means that there is a risk of the cancer lesions being hidden (masking risk). More robust and accurate risk models are expected to be developed.
For many women, the work on breast density measurement could change the course of their lives for the better. The urgency to establish international standard protocols in breast density measurement is imperative.
The research and medical community are called upon to heed the great need to promote breast density awareness. When breast density is able to indicate early signs of breast cancer, it has the potential to save many from the trauma of late diagnosis and its ensuing course of treatment.
Reference
This article is a summary from the publication (1) Kwan Hoong Ng and Susie Lau “Vision 20/20: Mammographic Breast Density and its Clinical Applications” Medical Physics 2015; 42: 7059-77 (DOI: 10.1118/1.4935141) and (2) Kwan-Hoong Ng, Cheng-Har Yip, Nur Aishah Mohd Taib, et al “Standardisation of clinical breast-density measurement” Lancet oncology 2012; 13: 334-6.
1 White J. Breast Density and Cancer Risk: What Is the Relationship? JNCI J Natl Cancer Inst.
2000; 92 (6): 443.
2 Boyd NF, Guo H, Martin LJ, et al. Mammographic density and the risk and detection of breast
cancer. N Engl J Med 2007; 356: 227–36.
3 Bradbury J. Breast density changes during menstrual cycle. Lancet 1998; 351: 1936.
4 Boyd NF, Martin LJ, Yaff e MJ, Minkin S. Mammographic density and breast cancer risk: current
understanding and future prospects. Breast Cancer Res 2011; 13: 223–34.
5 Boon D. Inherited mammographic density and breast cancer risk. Lancet Oncol 2002; 3: 646.
6 Brisson J, Brisson B, Maunsell E, Berube S, Robert J. Tamoxifen and mammographic breast
densities. Cancer Epidem Biomar Prev 2000; 9: 911–15.
7 Kolb TM, Lichy J, Newhouse JH. Comparison of the performance of screening mammography,
physical examination, and breast US and evaluation of factors that influence them: an analysis
of 27,825 patient evaluations. Radiology 2002; 225(1):165-75.
Acknowledgement
The UMMC breast density research team consists of radiologists (Prof Yang Faridah Abdul Aziz, Prof Kartini Rahmat, Assoc Prof Anushya Vijayananthan, Dr Farhana Fadzli, Dr Shaleen Kaur, Dr Chan Wai Yee); surgeon (Prof Nur Aishah Mohd Taib); medical physicist (Dr Susia Lau).
Contact Information
Professor Kwan Hoong NG, PhD, DABMP
Department of Biomedical Imaging and University of Malaya Research Imaging Centre,
Faculty of Medicine, University of Malaya, Kuala Lumpur
[email protected]