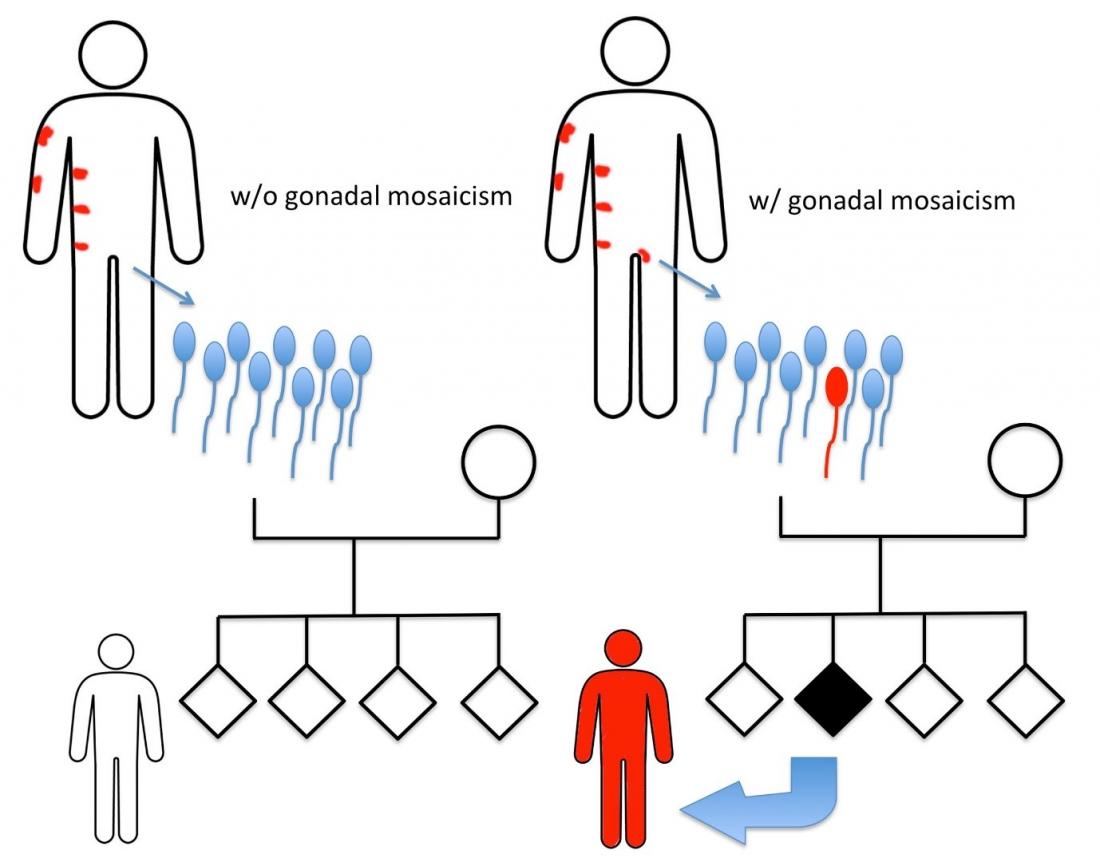
Epidermolytic nevus (EN) is visible as patches of thickened skin over small areas of the body. Mutations in genes encoding the skin proteins keratin 1 or keratin 10 are responsible for EN, but these mutations only occur in some cell populations of the body, including those of skin lesions, so they are known as mosaic. When the causative mutation occurs in germ cells, it is known as gonadal mosaicism. Birthmarks are not usually inherited because sperm cell genes are rarely mutated. However, when inheritance does occur, the children develop skin symptoms identical to their affected parent but covering their entire body.
Nagoya, Japan – Birthmarks can be caused by an overgrowth of cells in the top layer of skin, as in the case of epidermolytic nevus (EN), which is visible as patches of thickened skin over small areas of the body. Mutations in genes encoding the skin proteins keratin 1 or keratin 10 are responsible for EN, but these mutations only occur in some cell populations of the body so they are known as mosaic. Birthmarks are not usually inherited because the genes of sperm and cells are rarely mutated. However, when inheritance does occur, the children develop skin symptoms identical to their affected parent but covering their entire body.
Research at Nagoya University in collaboration with Juntendo University Urayasu Hospital has led to the identification of one such case of EN in a father that was transmitted to his daughter as a sperm cell (germline) mutation, resulting in the more widespread skin disorder epidermolytic ichthyosis (EI), which affects the whole body. The study was reported in the Journal of Investigative Dermatology.
EI symptoms are obvious from birth as skin redness and blistering that completely covers the body. This worsens over time, with the skin becoming scaly and thickened. Nagoya University researchers clinically diagnosed EI in a 2-year-old Japanese girl, and confirmed her diagnosis with the detection of a mutation in the gene encoding keratin 10.
The girl’s father had small patches of thickened skin on his hand, abdomen, and groin, affecting just 0.5% of his body surface. “We took a skin sample from one of these areas and identified the identical keratin 10 mutation that we detected in his daughter,” co-author Yasushi Suga says. “This confirmed that the same mutation was causative of EN in the father and had been transmitted to the daughter as EI.”
The parents of the girl wanted to know the likelihood of their future children being affected by EI, so the research team used a highly sensitive DNA sequencing technique to reveal that 3.9% of the father’s semen carried the mutation. However, determining the exact risk of disease transmission requires consideration of the effect that the mutation has on the sperm’s ability to fertilize an egg.
“Symptoms of mosaic inherited skin disorders are highly visible so diseases can be identified before the birth of affected children, unlike genetic diseases that don’t affect the skin,” corresponding author Michihiro Kono says. “This enables the risk of disease transmission to be determined, and couples to undergo genetic counseling.”