“Cancer metastasis is a complex process. Stiffness in tumours and the surrounding tissues is known to increase along with the tumour growth, which creates confined spaces or channel-like tracks of pores for tumour cell migration and metastasis in multiple cancer types. But the mechanism of this confined migration remains unclear,” said Professor Michael Yang Mengsu, Vice-President (Research and Technology) and Yeung Kin Man Chair Professor of Biomedical Sciences at CityU, who led the cross-institutional research. “We aim to deeply study the cancer metastasis mechanism and identify novel genes and proteins related to it.”
Hepatocellular carcinoma (HCC) is the most common type of the second leading cause of cancer death worldwide – liver cancer. Pancreatic ductal adenocarcinoma (PDAC) is another highly aggressive cancer with a five-year survival rate of less than 10%. Both of them have a typical feature of solid tumours with excessive extracellular matrix (ECM) deposition containing confined pores or channel-like tracks that enable cancer cell migration. So the team chose these two different cancer types as the study subjects.
Developing methods to study the migration mechanism
In collaboration with the Second Affiliated Hospital of Chongqing Medical University (CQMU), Professor Yang’s team first collected HCC and PDAC specimens for analysis from 153 and 63 patients, respectively, who had not received chemotherapy or radiotherapy before surgery. The team also obtained human liver cancer and pancreatic cancer cell lines from the National Institutes of Health in the USA.
“The main challenge was to simulate the complex cancer microenvironment,” explained Professor Yang. “But there is a lack of study models for cell migration in confined environment. So we developed a series of multidimensional platforms and 2D and 3D in vitro and in vivo models to comprehensively study the cell migration process.”
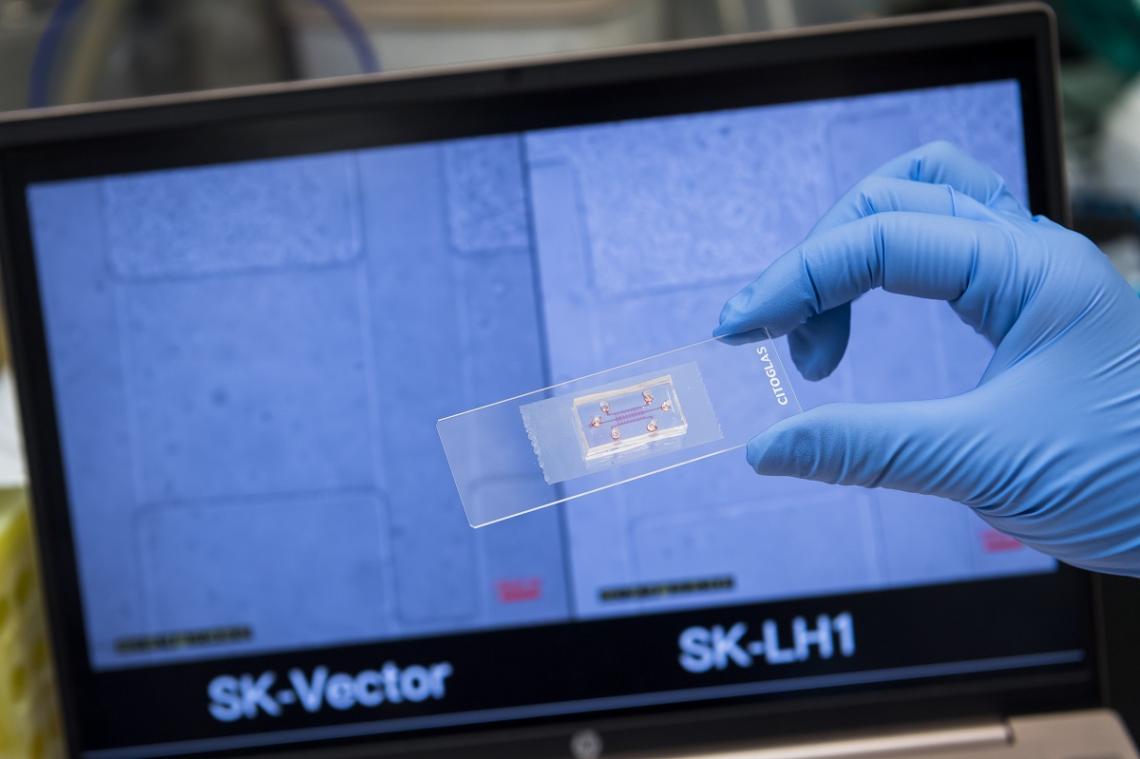
Microfluidic chips designed and fabricated by the team to mimic the in vivo environment. Credit: © City University of Hong Kong
These platforms and models include microfluidic chips for single-cell and collective cell migration, and hydrogels of various stiffness for 3D invasion assays to simulate the in vivo environment. The team also utilized next-generation sequencing (NGS) and liquid chromatography-mass spectrometry (LC-MS) to determine the differentially expressed genes and proteins in cancer tissues.
LH1 was strongly expressed in HCC tumour embolus.
Credit: © Yang, Z. et al. https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-0...
LH1 as a key factor in promoting confined migration of HCC and PDAC cells
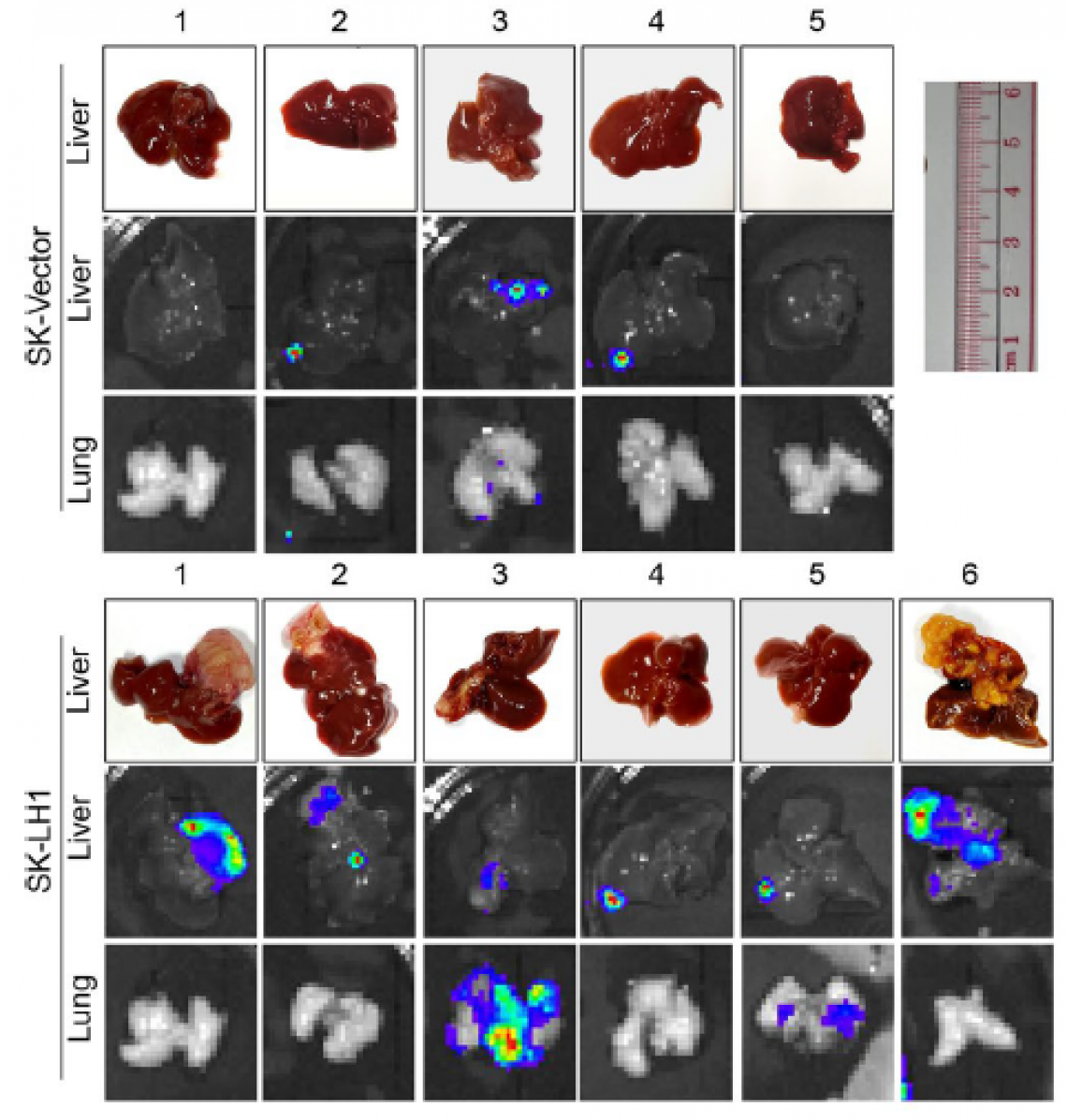
Based on the transcriptomic analysis with NGS and proteomic analysis with LC-MS, the team identified a protein called lysyl hydroxylase 1 (LH1) as one of the most significantly overexpressed proteins in HCC tissues. The microfluidic chips and 3D invasion models they developed demonstrated LH1’s capability to promote confined migration at multidimensional levels, including speed and invasion capacity of HCC and PDAC cells. The effects can be suppressed by knocking down the expression of LH1.
The research team observed that the LH1 overexpressing group had significantly larger tumours in the liver of a mice model with liver orthotopic injection. Credit: © Yang, Z. et al. https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-0...
They also demonstrated that LH1 could bind and stabilize Septin2 (SEPT2), a protein that plays an essential role in preparing the cells for high mechanical migration demand, to enhance the formation of an actin network. The actin network is the most dynamic element of the cytoskeleton, is distributed throughout the cell cytoplasm, and controls cell mechanics and motility. Thus, the enhanced formation of the actin network can promote the confined migration and metastasis of HCC and PDAC cells.
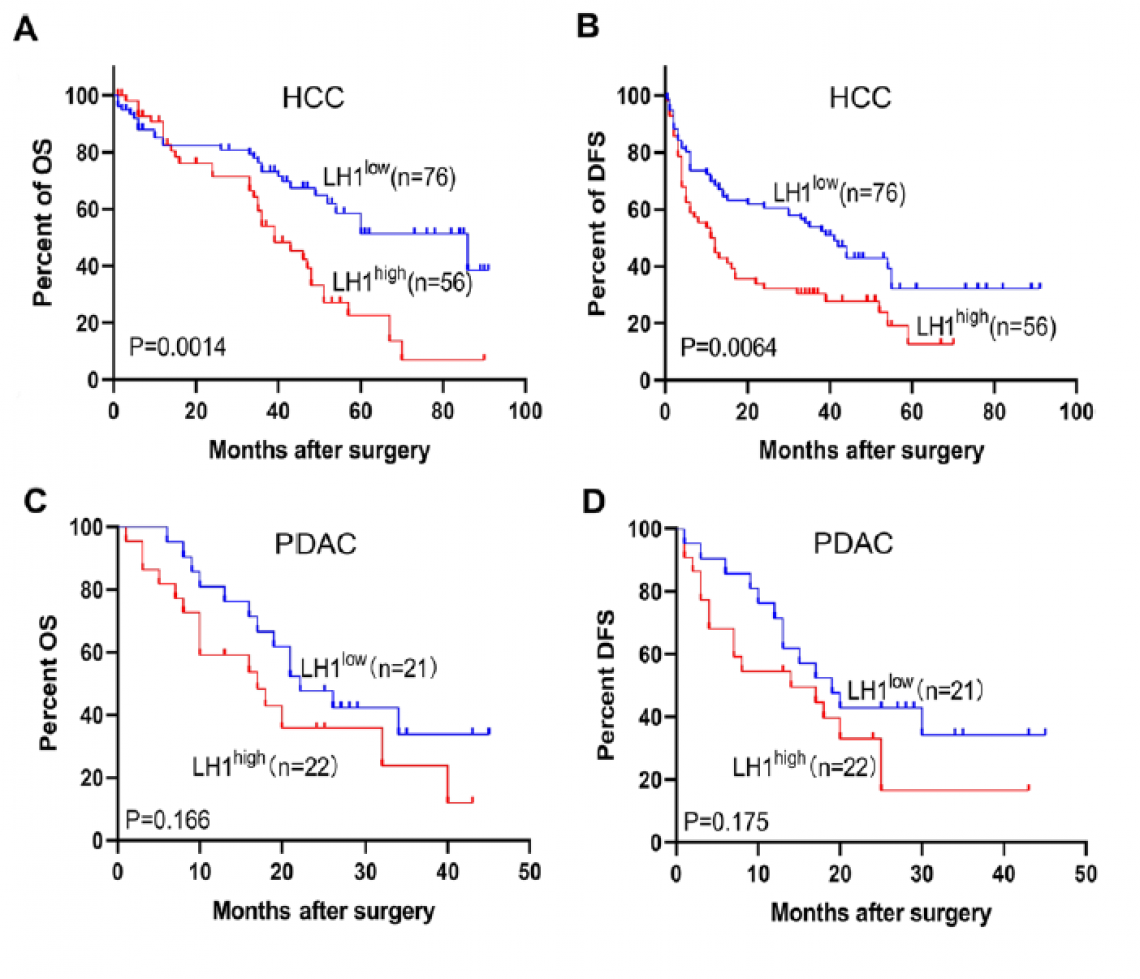
The figures show that patients with high LH1 protein expression level had a shorter overall survival and disease-free survival time with HCC (fig. A&B) and PDAC (fig. C&D).
Credit: © Yang, Z. et al. https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-0...
High LH1 expressed level results in poor prognosis for cancer patients
The research team also analysed the correlation between LH1 and prognosis (i.e. the development of disease and chance of relapse) of HCC and PDAC patients. The clinical samples showed that patients with higher LH1 expression, along with poor prognosis, had only half of the survival rate of the low LH1 expression group.
Moreover, HCC and PDAC patients with high LH1 expression experienced a shorter overall survival time from the date of diagnosis to death of 39 and 17 months, respectively, compared to 86 and 22 months for patients with a lower level of LH1. Also, their disease-free survival time from primary treatment to relapse of the disease was 11.5 and 14 months, respectively, compared to 41 and 19 months for patients with a lower LH1 level.
“The platforms and methods we developed provide a unique approach to study the confined migration of cancer cells,” said Professor Yang. “We demonstrated that LH1 promotes confined migration and metastasis of cancer cells by stabilising SEPT2, and that high LH1 is associated with poor prognosis of HCC and PDAC patients. The findings are expected to provide a potential new target for cancer diagnosis and drug development.”
The findings were published in the leading peer-reviewed cancer-related scientific journal Molecular Cancer, under the title “Lysyl hydroxylase LH1 promotes confined migration and metastasis of cancer cells by stabilizing Septin2 to enhance actin network”.
Professor Michael Yang Mengsu, Vice-President (Research and Technology) and Yeung Kin Man Chair Professor of Biomedical Sciences (3rd from right), Ms Eileen Yang Zihan, PhD student in Professor Yang’s research group (4th from right), and other members of the research team at CityU.(credit: © City University of Hong Kong)
The first author is Ms Eileen Yang Zihan, a PhD student in Professor Yang’s research group. The corresponding authors are Professor Yang and Dr Zhou Zhihang, a former visiting scholar in Professor Yang’s group, and currently Associate Professor at the Second Affiliated Hospital of CQMU. The multi-institution team consists of researchers from the Department of Biomedical Sciences and the Tung Biomedical Sciences Centre at CityU, the Department of Gastroenterology and the Department of Pathology at the Second Affiliated Hospital of CQMU, the Precision Diagnostic and Therapeutic Technology Centre of CityU Futian Research Institute, and The Hong Kong Polytechnic University.
The research was supported by Hong Kong Research Grants Council, the National Natural Science Fund, and theLoop Shenzhen-Hong Kong Science and Technology Innovation Cooperation Zone Shenzhen Park Project.