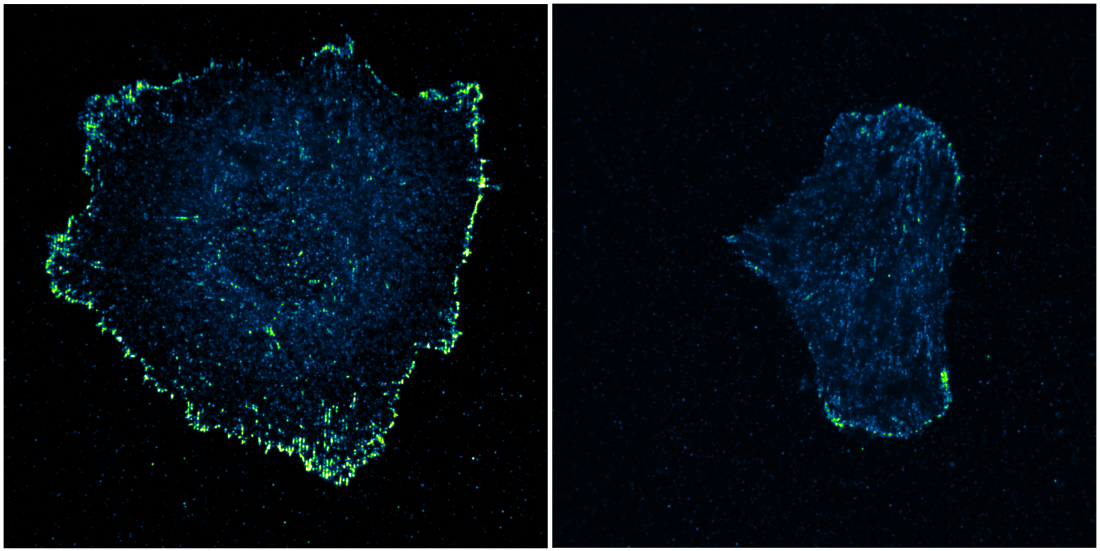
Image of fibroblast cells grown on artificial nanofibres with differential patterning and spacing. When the nanofibres were closely spaced (left panel), cells easily form stable focal adhesions (seen as bright green dots along the cell boundary) leading to increased cell spreading and migration. On the other hand, when the spacing between the nanofibres was increased, (right panel), cells have trouble forming strong focal adhesions and subsequently spread to a lesser extent.
Researchers from the Mechanobiology Institute (MBI) at the National University of Singapore have shown that cells can attach to the fibrous protein meshwork that surrounds them only if the fibres are spaced close enough. The team’s findings, which can explain the abnormal motility patterns displayed by cancer cells, were published in the science journal Nature Materials in September 2019.
The human body is made up of around a trillion cells. These cells stick to a supportive surface underneath (also known as matrix) as well as to the cells next to them.
Cell sticking forms the basis for the organisation of tissues, organs, and organ systems in multicellular organisms. Cells sticking to the matrix is essential for controlling important cell functions, including how much they move within the tissue. When this sticking is partially or completely lost, cells start to move erratically, a characteristic that is hallmark of metastatic cancers.
Cells also use sticking to know more about the physical and chemical nature of the matrix. Any disruption to how this information is relayed can lead not just to cancers, but many other serious diseases including those that affect the heart and the nervous system.
Hence, cell sticking can have major implications on health and diseases. This has spurred research on the topic, and over the past few decades many labs from all around the world have investigated the proteins and mechanisms involved in cell sticking. Researchers today now know that proteins at the cell periphery physically interact with proteins found in the matrix and these molecular connections basically are the attachment points between the cell and the matrix.
In the matrix, proteins mainly exist as fibres, which are arranged into a complex meshwork. Binding of the cell periphery proteins to this fibrous meshwork is a complex process, as several factors, such as the composition, density, and pattern of fibres can play a role.
In order to understand this complexity, imagine yourself walking on a net. The ease with which you can walk will mainly depend on how close the ropes of the net are: in essence, they must be patterned so as to provide sufficient footholds for support.
This analogy, when applied to cells, led to the hypothesis that cell periphery proteins would bind to matrix fibres and initiate cell sticking only if the fibres are arranged in a manner that offers sufficient footholds for binding. The study carried out in the Sheetz Lab at MBI investigated this important idea by trying to find out if fibre spacing could actually control cell sticking.
The study was led by MBI’s Senior Research Fellow Dr Rishita Changede together with Principal Investigator Professor Michael Sheetz, along with collaborators from Columbia University. The team created artificial nanometre-sized fibres and arranged them in various 1D or 2D patterns that differed in the spacing between the fibres; these artificial fibres mimicked protein fibres found in the matrix. They then grew connective tissue cells known as fibroblasts on these artificial fibres and used advanced microscopes to compare the extent of cell sticking to the various patterns.
Based on their observations, the researchers drew one important conclusion – the spacing between the fibres is crucial for efficient cell sticking. Cells can stick strongly to the matrix when adjacent fibres are spaced closer than 160 nanometres apart. If this spacing was increased, cells cannot stick to the fibres.
To understand how diseases like cancers evolve is like trying to solve one complex jigsaw puzzle with several pieces still missing. By showing how fibre spacing could control cell sticking, the study unravels yet another important piece of the puzzle relating to cell adhesion and movement and allows scientists to better understand what could be going wrong and identify molecular pathways that could be used as therapeutic targets for treating these diseases.
From a clinical perspective, the critical role of fibre spacing described here can be applied to design customised artificial surfaces for use in regenerative medicine. This breakthrough medical technology enables the regeneration of damaged cells, tissues, or organs for therapeutic use. Controlling fibre spacing on artificial surfaces could optimise cell sticking and growth, enhancing the regeneration efficiency of these cells. The higher yield of restored, healthy cells thus obtained could be used for the treatment of patients with life-threatening or debilitating health conditions.