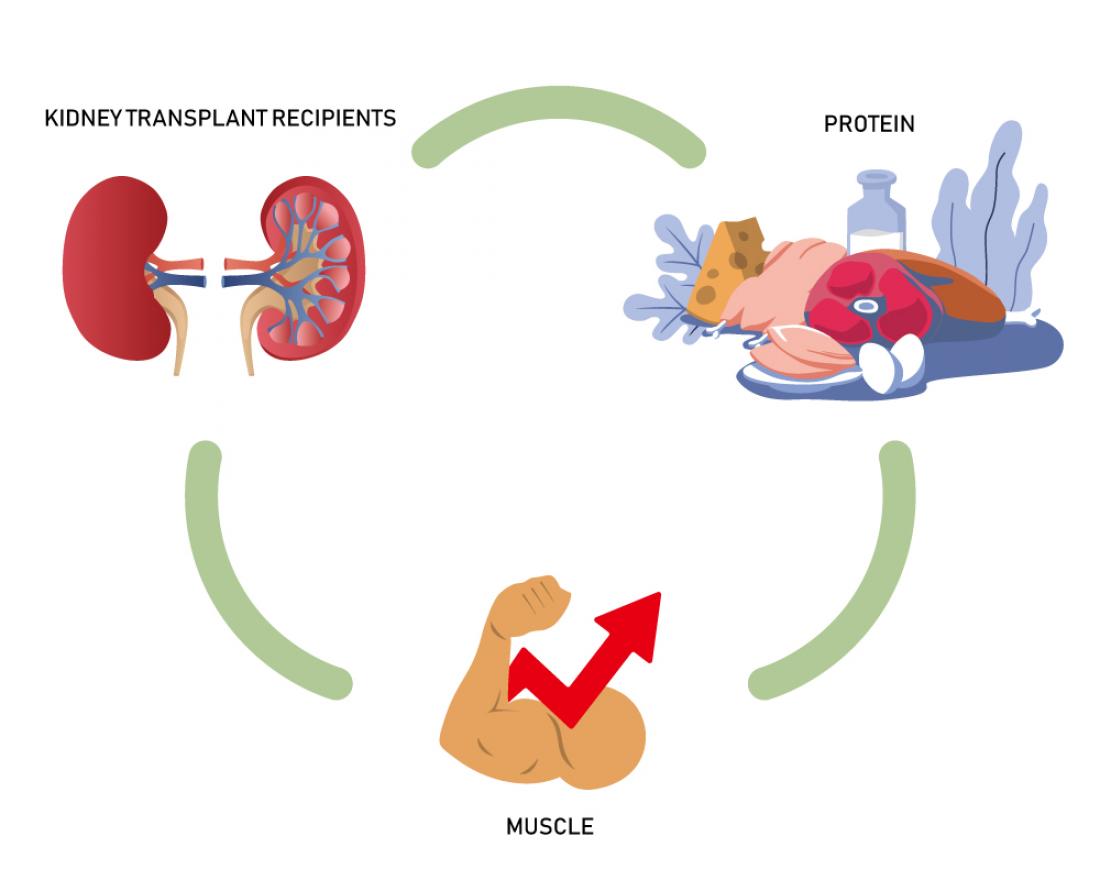
OMU scientists found that changes in skeletal muscle mass were positively correlated with protein intake, suggesting the necessity of adequate protein intake to improve muscle mass after kidney transplantation.
Osaka, Japan – Conventional wisdom holds that low protein intake is essential for kidney disease patients. However, scientists from Osaka Metropolitan University demonstrated that it might not always be the case with their recent study on the relationship between protein intake and skeletal muscle mass in kidney transplant recipients. Their findings were published in Clinical Nutrition.
Chronic kidney disease patients are known to have induced sarcopenia due to chronic inflammation, hypercatabolism, decreased nutrient intake, and decreased physical activity associated with impaired kidney function. Recovery of renal function due to successful kidney transplantation is able to correct or improve many of those physiological and metabolic abnormalities. As a result, kidney transplant recipients increase skeletal muscle mass after kidney transplantation. Since excessive protein intake worsens kidney function, it is commonly believed that patients with chronic kidney disease, including kidney transplant recipients, should limit protein intake to protect their kidneys. On the other hand, it has been suggested that severe protein restriction may worsen sarcopenia and adversely affect prognosis.
Since nutrition and exercise therapy are recommended to improve sarcopenia, protein intake is suspected to relate to recovery of skeletal muscle mass after kidney transplantation. However, few studies have examined the relationship between skeletal muscle mass and protein intake in kidney transplant recipients.
Responding to this gap, the research group led by Dr. Akihiro Kosoku, Dr. Tomoaki Iwai, and Professor Junji Uchida at the Department of Urology, Graduate School of Medicine, Osaka Metropolitan University investigated the relationship between changes in skeletal muscle mass—measured by bioelectrical impedance analysis—and protein intake, which was estimated from the urine collected from 64 kidney transplant recipients 12 months after kidney transplantation. The results showed that changes in skeletal muscle mass during this period were positively correlated with protein intake, and that insufficient protein intake resulted in decreased muscle mass.
Dr. Iwai and Dr. Kosoku commented, "To improve the life expectancy of kidney transplant recipients, further research is needed to clarify the optimal protein intake to prevent either deterioration in kidney function or sarcopenia. We hope that nutritional guidance, including protein intake, will lead to improved life expectancy and prognosis.”
###
About OMU
Osaka Metropolitan University is a new public university established by a merger between Osaka City University and Osaka Prefecture University in April 2022. For more science news, see https://www.upc-osaka.ac.jp/new-univ/en-research/, and follow @OsakaMetUniv_en, or search #OMUScience.