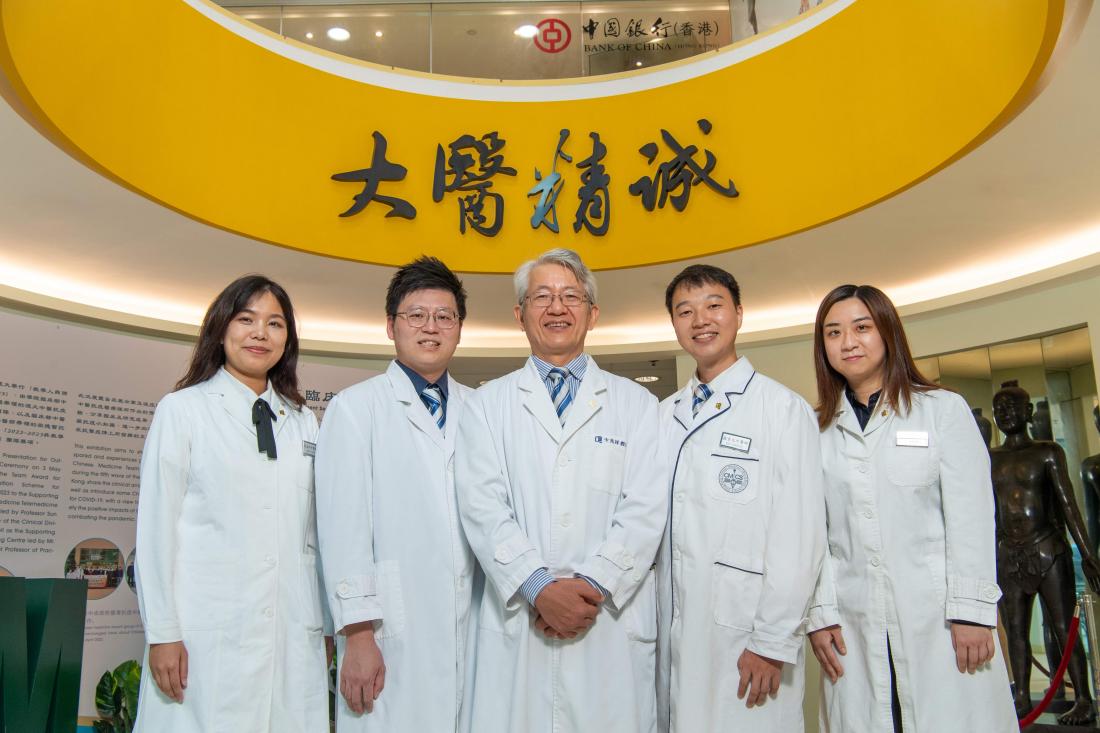
Professor Bian Zhaoxiang, Director of the Clinical Division at HKBU’s School of Chinese Medicine (middle), together with his research team members Mr Cheung Chun-hoi, Associate Director of the Clinical Division (2nd left); Dr Zhang Jialing, Postdoctoral Fellow of the Centre for Chinese Herbal Medicine Drug Development (1st left); Mr Luo Jingyuan and Wong Hoi-ki, PhD students (2nd and 1st right) of SCM at HKBU, analyse patient statistics to deepen the medical community’s understanding of the symptoms during the early and middle stages of COVID-19 infection as well as the post-COVID syndrome.
The School of Chinese Medicine at Hong Kong Baptist University (HKBU) found that 55% of the patients who sought medical treatment from the “HKBU Chinese Medicine Telemedicine Centre Against COVID-19” during the fifth wave of the COVID-19 pandemic continued to experience at least one long COVID symptom for six months to a year after diagnosed with an infection. The most common symptoms are fatigue, brain fog and cough.
The study also revealed that patients who took Chinese medicine after COVID-19 infection took a shorter time to test negative in rapid tests, and experienced significant symptom relief compared to patients who did not take Chinese medicine.
The research findings have been published in a number of papers in international academic journals including the Journal of Medical Virology and The American Journal of Chinese Medicine.
HKBU established the “HKBU Chinese Medicine Telemedicine Centre Against COVID-19” in 2021 during the fifth wave of the COVID-19 pandemic in Hong Kong to provide free telemedical services for COVID-19 patients. Making reference to the treatment protocols and clinical experiences in Mainland China, the expert team of HKBU’s School of Chinese Medicine formulated the “Chinese Medicine Clinical Guidelines for COVID-19 in Hong Kong” as the University’s clinical diagnosis and treatment standards for COVID-19. The Telemedicine Centre follows the guidelines to provide diagnosis, treatment, and prevention services to COVID-19 patients, close contacts, and caregivers.
Coughing is the most common early symptom of infection
The HKBU research team led by Professor Bian Zhaoxiang, Director of the Clinical Division at the School of Chinese Medicine, conducted a retrospective study using patient statistics collected by the Telemedicine Centre during the fifth wave of the pandemic. The team analysed the symptoms in the first four weeks of about 13,000 patients who were infected with COVID-19 from mid-March to early May in 2022 and underwent home isolation.
The results showed that 93% of patients experienced at least one symptom. The most common symptoms during the first week of infection were cough (91%), sputum (75%), dry throat (50%) and sore throat (44%). 17% of patients still had these symptoms four weeks after infection. Although the symptoms gradually subsided over time, the prevalence of fatigue increased.
Chinese medicine accelerates viral clearance
Among this batch of patients, the research team selected 311 patients who had taken Chinese medicine for five days within 10 days after diagnosis, and another 311 patients who had not taken any Chine medicine during the same period to evaluate the efficacy of Chinese medicine.
The results showed that patients who took Chinese medicine within 10 days after COVID-19 infection needed an average of seven days to test negative in rapid tests, and experienced an average of four symptoms, which were significantly milder compared to patients who didn’t take Chinese medicine. The average time to test negative for patients who did not take Chinese medicine was eight days, and they experienced an average of 11 symptoms. The results show that Chinese medicine is an effective treatment for COVID-19 infection.
Over half of the patients experience long COVID after six months
The research team conducted a follow-up telephone survey from November 2022 to January 2023 with 6,242 COVID-19 patients who sought medical consultation at the Telemedicine Centre between December 2021 and May 2022 to understand their symptoms and risk factors after six months to a year of infection.
The study found that 55% of patients still experienced at least one long-term symptom, i.e. “long COVID” or “post-COVID syndrome”. The most common symptoms were fatigue (36%), brain fog (34%) and cough (31%). Furthermore, females, middle-aged persons, obese people, those with comorbidities such as ophthalmology or otorhinolaryngology diseases, digestive system diseases, respiratory diseases, hyperlipidemia and cardiovascular diseases, and patients with more initial symptoms were more likely to develop long COVID. However, there was no significant correlation between taking three or more doses of vaccine and the occurrence of long COVID.
Professor Bian said: “HKBU established the Telemedicine Centre during the COVID-19 outbreak to provide free treatments for COVID-19 patients. We analysed the Centre’s data to deepen the medical community’s understanding of the symptoms during the early and middle stages of COVID-19 infection as well as the post-COVID syndrome. It allows the public to understand the effectiveness of Chinese medicine in treating COVID-19. The study also shows that the tele-services of Chinese medicine can be an important component of Hong Kong’s healthcare and disease prevention system.”
-End-