Overview of the HIS structure
Introduction
Application of IT to medical care has the following two aspects: (1) improvement and increased efficiency of medical services and (2) contribution to the progress of medicine. Its negative aspects are security-related issues for personal medical information.
An example of the improvement and increased efficiency of medical services is the use of computers for the control of various medical devices as well as the registration of patients and billing for hospital charges which has already been introduced in hospitals and other institutions. Furthermore, such computers can be connected to those on the desk of physicians using the hospital information system (HIS) to streamline medical activities.
Spread of electronic receipts
The billing for hospital charges includes the following work: 30% of medical service charges are collected from patients, and for the remaining 70%, a bill (also called as a receipt) is sent to the health insurance agency of each patient. In Japan, electronic receipts that handle these receipts electronically were standardized by the ORCA project of the Japan Medical Association in 2002, and a relevant software program was released free of charge as open source software. As a result, electronic receipts spread rapidly, and as of November 2011, 99.7% of bills from hospitals (with not less than 20 inpatient beds) were handled online through a network in Japan.
Hospital information system and electronic medical records
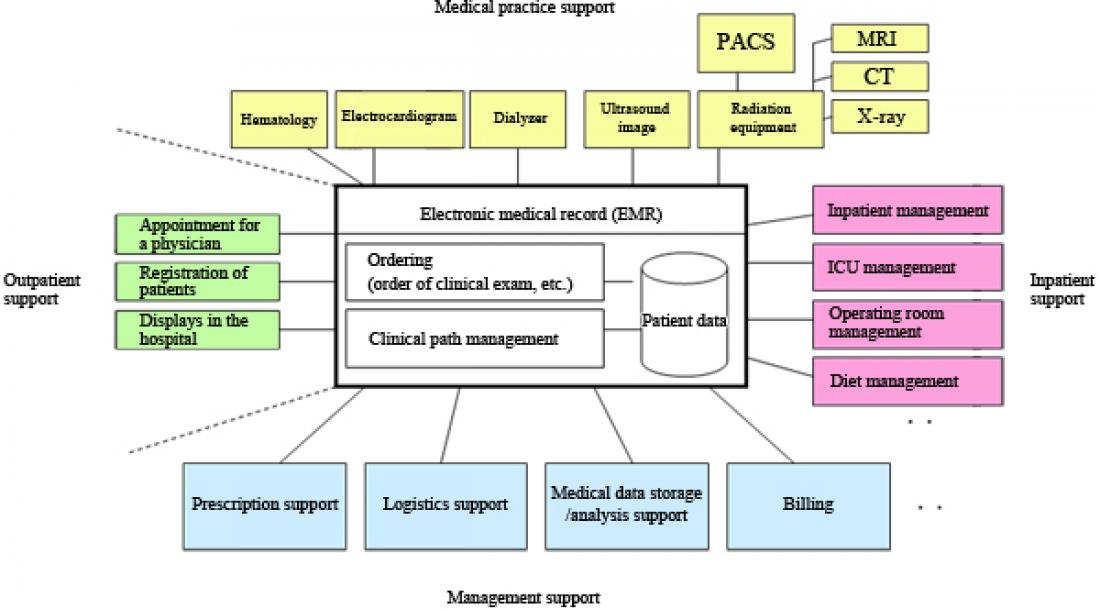
A key to actualizing the HIS is electronic medical records (EMRs) as illustrated in Fig. 1.
There is no widely used standard for EMRs as with the ORCA for electronic receipts. Thus, EMRs have been introduced in only 23.6% (in 2008) of major hospitals with no fewer than 200 beds as presented in Table 1. The situation of EMR introduction is similar in most Western countries.
Table 1 Situation of EMR introduction
2002 2005 2008
Major hospitals
(with no fewer than 200 beds) 1.5 10.1 23.6
All hospitals
(with no fewer than 20 beds) 1.2 6.9 13.2
Source: Survey of Medical Institutions, Ministry of Health, Labour and Welfare (2002, 2005, and 2008)
Standardization of EMRs
The reasons include the followings: software programs are expensive as EMR system providers have to build all systems on their own due to the lack of standards and the software is thus not reused; and there is no interoperability with other institutions such as hospitals, clinics, and pharmacies. If EMRs are standardized as with electronic receipts and a software system based on the standard is released free of charge on the Internet as an open source, EMRs will be introduced rapidly.
An international standard called openEHR, whose standardization is in progress mainly in Europe, is likely to be the shortest way to accelerate introduction. The major reason is that the standard does not standardize EMRs themselves, but it standardizes various basic medical concepts as archetypes and EMRs consist of a combination of such archetypes. This allows scalability to respond flexibly to changes in medical services and progress in medicine. Furthermore, it was already standardized by the ISO in 2009 (ISO13606) and a software program based on the standard can be downloaded freely from the Internet as an open source.
The other major international standard for EMRs is Health Level 7 (HL7), whose standardization is in progress mainly in the U.S. and also broadly around the world. It is noteworthy that clinical document architecture (CDA) is standardized in HL7. Standardization took place in 2009 jointly by the ISO and HL7 (ISO/HL7 27932: 2009). Based on this, the Ministry of Health, Labour and Welfare standard “HS008 Patient Referral Document (Electronic Referral Letter)” was established in March 2010 in Japan.
Global standardization of EMRs does not only improve and streamline medical services—there are also expectations that (1) the results of various IT-based medical studies will be communicated broadly to the world and (2) collected standardized medical data will enable evidence-based medicine, contributing to further progress of medicine.
Security
When IT is applied to medicine, security measures to handle personal health information are important. For this purpose, solutions are being discussed widely around the world. The following are the key issues particularly in medicine in addition to legal and technical security measures that have already been taken.
(1) Physicians and other medical professionals who can have access to personal health information along with patients should be identified, and for each person, the scope of information to which he or she has access (for example, all information or limited only to insurance-related information) and the authority only for information reading or also for writing should be specified.
(2) The scope within which the information can be used as reference data for medical research should be provided as necessary as well as sufficient information for medical research after masking information that can identify individuals.
Conclusion
The application of IT to medicine will offer great convenience as with automobiles, but it also carries a large risk (accidents, security). From this standpoint, it is expected to gather opinions and wisdom carefully from a wide range of relevant people for further progress.