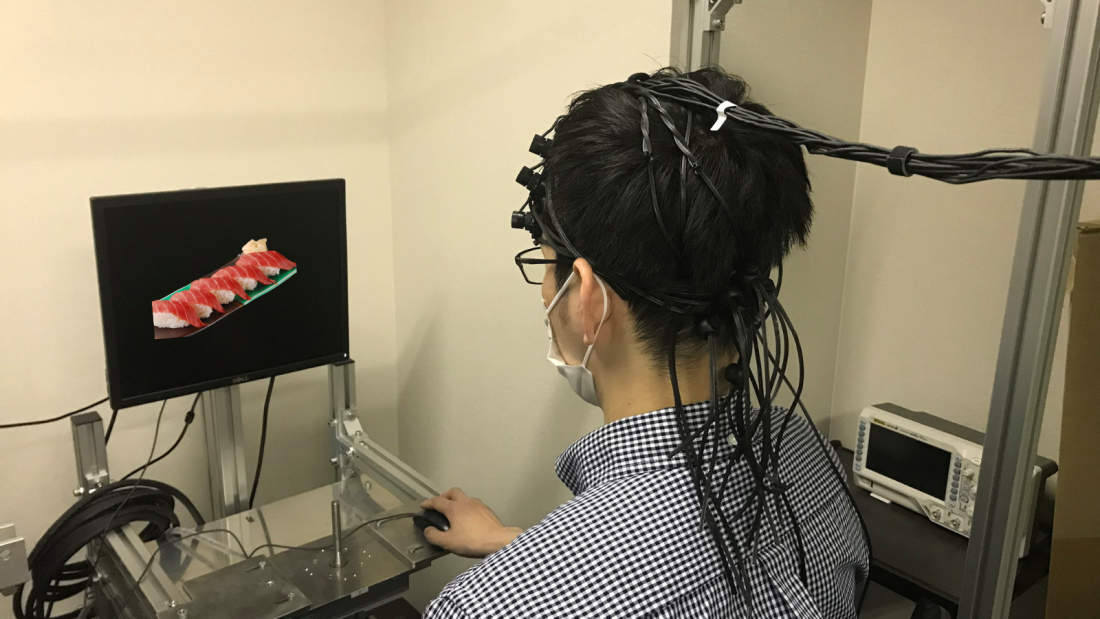
Monitoring participants’ brain activity while viewing food images. Patients with functional dyspepsia experience mental stress watching images of food.
Patients with a type of chronic indigestion called functional dyspepsia experience abdominal discomfort without having obvious physiological or biochemical causes. The condition shares similarities with irritable bowel syndrome (IBS). Researchers at Kawasaki Medical School in Japan have used brain signals gathered from the surface of the head to suggest that patients with functional dyspepsia experience mental distress simply by watching images of food they dislike.
Functional dyspepsia and IBS are examples of disorders of gut-brain interaction (DGBI), which can have a long-term negative impact on patients’ social and mental health, leading to decreased quality of life and reduced productivity at work. Each condition affects between 2% and 3% of the population of Japan.
“Our research reveals that the patients’ suffering in functional dyspepsia is real, despite other people often having a lack of empathy for this condition, as there is no evidence of what could be causing their problem,” says clinical researcher Ryo Katsumata of the Kawasaki Medical School team.
Patients’ preferences for food were analyzed, revealing significantly reduced preference for fatty foods in the group with functional dyspepsia.
Participants’ brain activity while viewing food images was then detected using functional near-infrared spectroscopy (fNIRS). This uses an array of scalp-mounted detectors to assess brain activity by monitoring the levels of oxygen-carrying hemoglobin in the outer layer of the brain called the cerebral cortex. Increased oxygen delivery by hemoglobin is presumed to reflect increased brain activity in the regions involved.
Patients with functional dyspepsia showed lower scores for food images, but had similar scores for animal images compared to healthy patients.
The study compared the brain activity of patients with functional dyspepsia or IBS with the activity of healthy control subjects. When presented with images of a variety of foods, patients with functional dyspepsia had significantly higher brain activity in the left anterior part of the cortex than those with IBS or healthy controls. No significant difference was detected between the response of patients with IBS and the healthy control subjects, leading the researchers to draw conclusions only about functional dyspepsia.
The researchers interpret their results as evidence of a strong reaction of mental stress in the patients with functional dyspepsia when viewing any types of foods, but especially foods they dislike. It certainly provides convincing evidence of different reactions to viewing food images in their brains. The researchers conclude this supports the reality of patients’ symptoms and contradicts alternative views that can lead to lack of empathy for patient suffering.
“We now hope to advance this research by using artificial intelligence to construct an fNIRS process that can support the diagnosis of functional dyspepsia,” says Katsumata. “We also hope to investigate IBS further.”
For more information, contact:
Associate Professor Ryo Katsumata
Email: [email protected]
Personal blog: https://gutbraininteraction.blogspot.com/
Kawasaki Medical School
Website: https://k.kawasaki-m.ac.jp/
Reference: Katsumata, R., Hosokawa, T., Manabe, N. et al. Brain activity in response to food images in patients with irritable bowel syndrome and functional dyspepsia. J Gastroenterol (2023). https://doi.org/10.1007/s00535-023-02031-5